Abstract
We have previously reported on the challenges of treating AML in India, the major challenge being the cost of treatment (Chepsy et al. BJH 2015). With conventional treatment of AML it is recognized that the major part of this cost is not related to the cost of the individual chemotherapeutic drugs, but rather from the high cost of supportive care to take patients through repeated cycles of prolonged neutropenia induced by conventional chemotherapy. In contrast with arsenic trioxide (ATO) based regimens in acute promyelocytic leukemia (APL), when expensive patented 'innovator' ATO was used, the reported 3 year direct pharmacy cost of drugs was higher with an ATO+ATRA regime compared with a conventional ATRA+chemotherapy regimen (Euro 46,700 Vs 6,700), though the cost of supportive care was a third of conventional therapy (Kruse M et al. PLoS One. 2015). There is limited data on the cost effectiveness of using generic ATO, as available in India, in the treatment of APL (10 mg vial costs US $7 in India versus US $ 676 in North America)
In a single center, retrospective study, 30 newly diagnosed APL (ND-APL) patients, treated with ATO and 16 relapsed APL (R-APL) patients, treated on a phase II trial with a ATO based regimen followed by an autologous stem cell transplant (regimens as previously reported by us; Mathews et al. Blood 2012 and Mathews et al. Blood 2016 abstract) were evaluated. In the absence of patients being treated at our center with a conventional ATRA+chemotherapy regimen (APL-CT) the cost of treatment for APL with such a regimen was assumed to be similar to the cost that would be incurred to treat a non-M3 AML patient at our center with a conventional AML chemotherapy schedule. Incremental cost effectiveness ratio was calculated using weighted costs with weighing factor obtained from survival data for 60 patients from our database for APL ATO group and from the AIDA 2000 trial for APL-CT group.
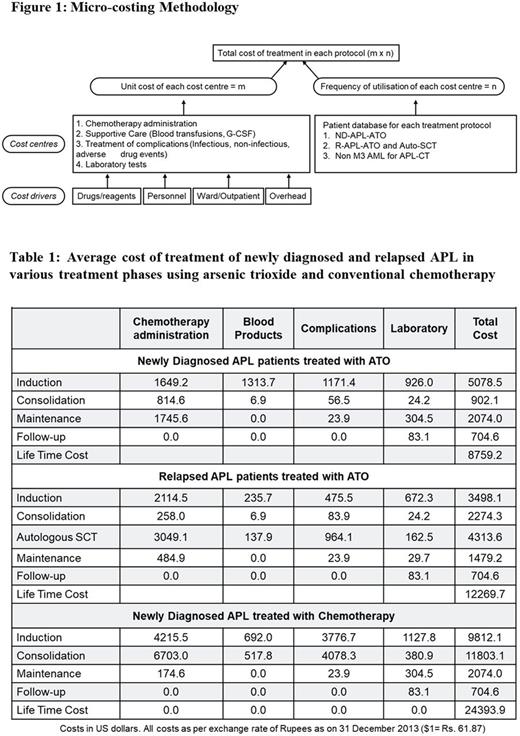
A three phase micro-costing method (figure 1) used four cost centers involved in providing patient care: (i) chemotherapy administration (ii) supportive care (iii) treatment of complications (iv) laboratory services. For each of these cost centers there were four cost drivers: (i) drugs / reagents (ii) personnel (iii) ward (iv) instruments / overheads. The actual cost of cost drivers was found out by micro-costing and summed up to obtain the unit cost of each cost center (m). Each time a patient used a cost center this unit cost would be incurred. Next, the frequency of utilization (n) of each cost center was found out from the patient database and multiplied by the unit cost of the cost center to obtain the total cost of treatment in each protocol (m x n) (For illustration and international comparison all cost were converted to US$).
In ND-APL patients, the mean cost of induction and consolidation was $5078.5±1581 and $902±212 respectively while in APL-CT it was $9812.1±3239 and $11803.1±4872 respectively (exchange rate 1 US$=61.87 Indian rupees). Our data illustrated that APL-CT group incurred higher costs mainly due to the greater duration of in-patient care that was required in this group and since they had higher rate of infectious complications (Table 1). During maintenance phase, in ND-APL, there were no in-patient stays and the entire chemotherapy was given on outpatient basis and the average cost was $2074±146 and the cost of following up these patients for an additional three years was $704.6±289. The mean lifetime cost of treatment of ND-APL using ATO was $8759.2±2078 while using APL-CT was $24393±5528. In R-APL patients, the total cost of re-induction and consolidation was $3498±1220 and $2274±372 respectively. The mean cost of an autologous-SCT was $4318±159. The average lifetime cost of treatment of relapsed APL patients using ATO based regimen followed by an autologous SCT was $12269.7±4915. The weighted cost per living for ATO and CT was estimated to be $12426 and $28330 respectively. The incremental cost effectiveness ratio showed ATO to be cheaper by $13359 for each life saved compared to conventional chemotherapy.
ATO based regimen in ND-APL and R-APL are associated with significant reduction in resource utilization and costs of treatment and is also cost-effective as compared to conventional ATRA+chemotherapy. With the world still debating the best treatment for APL, generic ATO based regimen offers a significant opportunity for resource constrained countries to treat all patients with a diagnosis of APL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal